In the rapidly evolving landscape of mental healthcare, technology is increasingly playing a pivotal role. Among the most discussed innovations is the integration of artificial intelligence (AI) into administrative tasks, particularly in generating therapy notes. While the promise of increased efficiency and reduced administrative burden is alluring, the ethical implications of using ai for therapy notes warrant careful examination. As practitioners, our primary commitment is to patient well-being, confidentiality, and the integrity of the therapeutic process. This article delves into the complex ethical considerations that arise when AI takes on the delicate task of documenting therapeutic interactions.
The Dual Promise and Perils of AI in Documentation
The appeal of AI-driven tools for therapy notes is undeniable. Therapists often spend a significant portion of their time on documentation, a task that, while essential, can detract from direct patient care and contribute to burnout. AI promises to streamline this process, potentially freeing up valuable time for clinicians to focus on their clients. Automated note-taking can ensure consistency, completeness, and adherence to regulatory standards, which in turn could lead to more accurate billing and improved data for research.
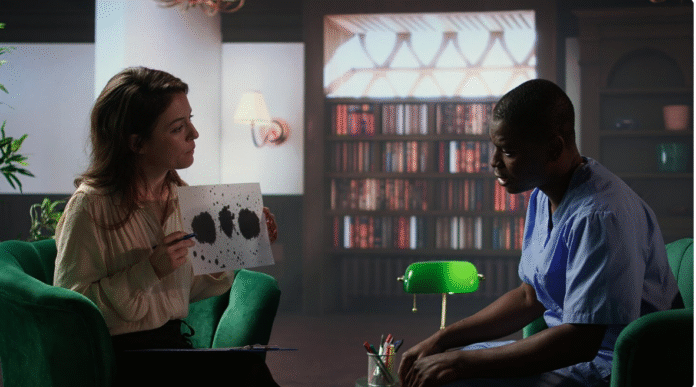
However, beneath this veneer of efficiency lies a labyrinth of ethical challenges. The very nature of therapy is deeply human, relying on nuance, empathy, and an understanding of unspoken cues. Can an algorithm truly capture the essence of a therapeutic session, or will it reduce complex human experiences to data points, potentially losing vital context and meaning?
Confidentiality and Data Security: A Paramount Concern
One of the most significant ethical hurdles when using ai for therapy notes is safeguarding patient confidentiality. Therapy notes contain highly sensitive and personal information. Any breach of this data can have devastating consequences for individuals, eroding trust in the therapeutic relationship and the mental health system as a whole.
AI systems, by their nature, require data to learn and operate. How is this data handled? Are robust encryption protocols in place? Who has access to the raw data and the generated notes? The potential for unauthorized access, data misuse, or even accidental leaks is a constant threat. Furthermore, the black box nature of some AI algorithms raises questions about transparency. Can we truly understand how AI processes information and generates summaries, or are we entrusting patient data to systems whose inner workings remain opaque? Ensuring compliance with regulations like HIPAA (Health Insurance Portability and Accountability Act) is non-negotiable, and providers must meticulously vet any AI solution for its security architecture and data governance policies.
Bias and Accuracy: The Reflection of Human Flaws
AI systems are only as unbiased as the data they are trained on. If the training data reflects societal biases – whether related to race, gender, socioeconomic status, or mental health diagnoses – the AI will inevitably perpetuate and even amplify these biases in its output. For example, an AI trained on predominantly Western or certain demographic data might misinterpret cultural nuances or expressions of distress from diverse populations, leading to inaccurate or incomplete notes.
The accuracy of AI-generated notes is another critical ethical point. While AI can transcribe spoken words, it may struggle with identifying sarcasm, non-verbal cues, or the subtle shifts in tone that convey significant emotional information. An AI might summarize a session factually but miss the underlying emotional narrative or the therapeutic breakthroughs that occurred. Relying solely on ai for therapy notes without rigorous human oversight could lead to notes that are technically correct but therapeutically misleading, potentially impacting treatment plans and patient outcomes.
Clinical Responsibility and Professional Judgement
Ultimately, the responsibility for patient care rests with the human therapist. When AI generates notes, where does the line of responsibility blur? If an AI misinterprets information, omits crucial details, or introduces errors, who is accountable? Therapists must maintain ultimate control and oversight over all documentation. AI should be viewed as a tool to assist, not replace, professional judgment.
Active Review and Editing: Therapists must thoroughly review and edit all AI-generated notes to ensure accuracy, completeness, and ethical soundness. This means not just a cursory glance but a deep engagement with the content to verify it accurately reflects the session.
Contextual Understanding: AI lacks the capacity for empathy and the intricate understanding of the therapeutic relationship. It cannot grasp the meaning behind a client’s silence or the unspoken dynamics in a session. The therapist’s role is to infuse the notes with this crucial human context.
Informed Consent: Patients have a right to know if AI is being used in their care, particularly in the documentation process. Transparent communication about the use of ai for therapy notes is essential for maintaining trust and upholding ethical standards of informed consent.
The Future of AI in Therapy Documentation: A Balanced Approach
The ethical challenges surrounding AI-generated therapy notes are significant, but they are not insurmountable. The path forward requires a balanced approach that leverages the benefits of AI while rigorously addressing its risks.
1. Prioritize Privacy and Security: Invest in AI solutions with robust encryption, anonymization capabilities, and clear data governance policies. Regular security audits are essential.
2. Ensure Transparency and Explainability: Favor AI models that are more transparent in their operations, allowing therapists to understand how suggestions are generated.
3. Implement Human Oversight: AI should always function as an assistant, with the human therapist retaining full responsibility for the final notes and clinical decisions.
4. Ongoing Training and Validation: AI models need continuous training on diverse, representative, and ethically sourced data to mitigate bias and improve accuracy.
5. Develop Ethical Guidelines: Professional organizations and regulatory bodies must collaborate to develop clear ethical guidelines and best practices for the use of AI in therapy documentation.
The integration of ai for therapy notes holds immense potential to transform mental healthcare by reducing administrative burdens and enhancing efficiency. However, this advancement must proceed with a profound respect for ethical principles, patient privacy, and the irreplaceable human element of therapy. By thoughtfully navigating these considerations, we can harness AI’s power to support, rather than undermine, the sacred trust between therapist and client.
Conclusion
The advent of AI in mental healthcare documentation presents a fascinating dichotomy: the promise of unparalleled efficiency versus a complex web of ethical dilemmas. While the allure of freeing therapists from the time-consuming burden of note-taking is strong, we must not lose sight of our fundamental responsibilities to our clients. Confidentiality, accuracy, bias, and the ultimate responsibility for clinical judgment are not negotiable. By adopting a cautious, ethical, and human-centered approach, we can ensure that AI serves as a valuable tool to enhance patient care, rather than compromise the integrity of the therapeutic process. The future of mental health documentation is undoubtedly intertwined with AI, but it is a future we must shape with deliberate ethical consideration and unwavering commitment to client well-being.
Author Bio:
This author is a seasoned mental health professional with over a decade of experience in clinical practice and healthcare technology. With a passion for integrating innovative solutions responsibly, they have contributed to numerous discussions on the ethical implementation of emerging technologies in therapeutic settings. Their work focuses on enhancing practitioner efficiency while upholding the highest standards of patient care and confidentiality.